Bridging the Rural Healthcare Gap:
The OptimalMD Health Partnership
A strategic proposal to enhance care delivery, reduce uncompensated costs, and improve health outcomes across rural communities through virtual-first healthcare integration.
Simulated Partnership

Rural and Community Hospitals
Community hospital systems specialize in strengthening rural healthcare systems through comprehensive services including:
Frontline Access To Care: Only Access Point
20% of Patient Pop vs. 10% of Doctors Available
Appx. $50 Billion in Uncompensated Care Annually
Level 5 ED Visit costs the hospital $500-$2,200
Significantly higher percentage of ALICE patients.
All services are tailored to improve operational efficiency and enhance patient outcomes in underserved areas.

Outpatient Overflow Support
Prevents many costs from reaching the ED by delivering turnkey and inclusive patient care for non-emergencies.
Reduces Nursing and Staff Workload and Cost
Compensates for Physician Shortages
Comprehensive Urgent and Primary care
Integrated Behavioral Health Services
Comprehensive Pharmacy Solution
Comprehensive Laboratory Solution
Specialist referrals and coordination
*High acuity and qualifed patients directed back to facility.
The Rural Healthcare Challenge
Limited Resources
Rural hospitals operate with thinner margins and fewer specialized resources than urban counterparts, making operational efficiency critical.
Access Barriers
Geographic isolation creates significant barriers to care, with patients often traveling long distances for basic services
Provider Shortages
Chronic staffing shortages limit service availability and put pressure on existing clinical teams, compromising care quality.
Financial Instability
High rates of uninsured patients and uncompensated care create unsustainable financial pressures, threatening facility closures.
The Financial Burden of Uncompensated Care (in Millions per Hospital)
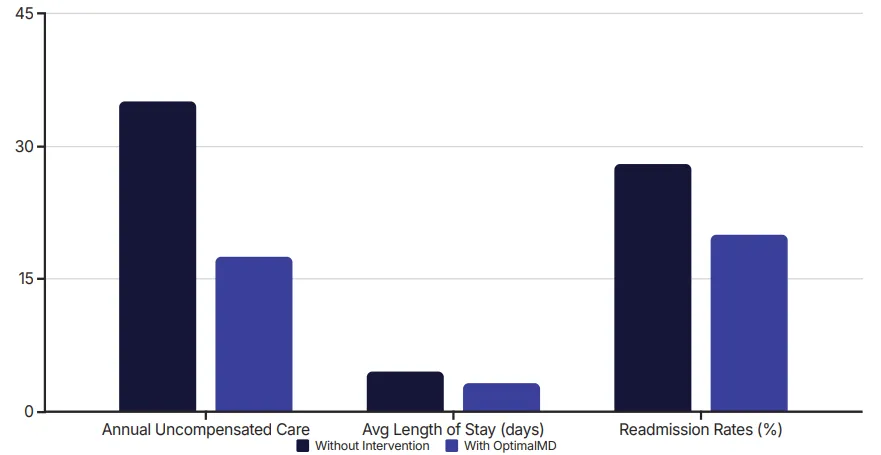
Current uncompensated care amounts to $25-$40M annually across RC's five hospitals, with a recovery rate of less than 20¢ per dollar billed to uninsured patients.
This represents 5-7% of net patient revenue 4 effectively erasing already thin rural margins and threatening long-term viability.
With the OptimalMD partnership, we project cost savings of $12-$20M per year by reducing uncompensated care by up to 50%
The OptimalMD Solution
Comprehensive Virtual Care
Unlimited Primary & Urgent care access
13+ specialty services including dermatology & behavioral health
1,100+ medications covered at $0 cost
Annual lab screenings & preventive care
24/7 doctor availability (17-minute average response)
Flat per patient fee or community memberships
No copays, no deductibles to the patient
Strategic Patient Flow Redesign
Non-resource patients are diverted to OptimalMD's virtual-first care model, addressing ~90% of healthcare needs without utilizing hospital resources.
Meanwhile, benefit-eligible patients are identified and redirected to RCH Health facilities for fully reimbursable services.
This dual approach creates a claims-free safety net for uninsured patients while protecting RCH's financial viability.
Benefits of Integration

Expanded Rural Access
24/7 virtual care eliminates geographic barriers and travel burdens for rural patients

Affordable Delivery
Flat-rate model eliminates surprise bills, deductibles, and copays for patients

Comprehensive Services
Virtual primary care, urgent care, behavioral health, and medications in one solution

Improved Workflow
Reduces non-emergency in-person visits, freeing up resources for critical care needs

Enhanced Recruitment
Attractive healthcare benefits help rural facilities attract and retain talent

Seamless Coordination
Integrated medication delivery, lab work, and care management reduce fragmentation
With a reported 95% patient satisfaction rate, OptimalMD complements RCH Health's operational expertise while addressing key challenges in rural healthcare delivery.
Proposed Collaboration Structure

Partnership Model
Strategic licensing/integration agreement customized for RCH Health's rural network
Deployment Options
Offered as an add-on service or fully integrated benefit within RCH's service portfolio
Structure
Referral-based, bundled pricing, or white-labeled service with RCH branding
Support Systems
Joint onboarding, marketing resources, and technical integration assistance
Performance metrics will track patient satisfaction, utilization patterns, cost savings through ER diversion, and overall operational efficiency improvements.
Implementation Roadmap
Joint Needs Assessment
Conduct market analysis of specific rural needs, volume forecasts, and population health gaps
Pilot Program
Launch targeted implementation at select RCH-affiliated rural facility to measure outcomes
Marketing & Education
Co-develop materials showcasing benefits for both patients and providers
Operational Integration
Establish seamless technical infrastructure for referrals and care coordination
Measurement & Expansion
Set KPIs and scale deployment based on pilot results across RCH network
Performance metrics will track patient satisfaction, utilization patterns, cost savings through ER diversion, and overall operational efficiency improvements.
Financial Impact
Reduction in uncompensated care
Increased revenue-positive cases
Overall cost efficiency gains
Operational Metrics
Reduced ED utilization
Decreased average length of stay
Lower readmission rates
Patient Experience
Access improvement scores
Patient satisfaction ratings
Care continuity measures
Summary: Creating a Sustainable Rural Health Model
For Rural Communities
Improved access to care regardless of location
Affordable, predictable healthcare costs
Comprehensive services including mental health
Sustained local hospital viability
All services are tailored to improve operational efficiency and enhance patient outcomes in underserved areas.
For OprimalMD
Reduced uncompensated care burden ($12-$20M/year)
Optimized resource utilization
Enhanced service offerings
Strengthened competitive position
By integrating OptimalMD's virtual care ecosystem with RCH Health's operational expertise, we can create a transformative healthcare delivery model that addresses the fundamental challenges facing rural healthcare.
Together, we can build a modern, efficient, patient-centered healthcare model that ensures the long-term sustainability of rural healthcare delivery.
